
Hormone Replacement Therapy (HRT): The Risks and Benefits Every Midlife Woman Should Know
Hormonal changes are inevitable in every woman’s midlife. With them often come hot flushes, night sweats, mood swings, sleep disturbances, and changes in energy or weight. The good news? Hormone Replacement Therapy (HRT) remains one of the most well-researched and effective treatments for managing these menopause and perimenopause symptoms. Understanding the facts - especially with the most recent evidence - is key to making the right decision for your own health. But, how do you know if it’s right for you?
What is Hormone Replacement Therapy?
Hormone replacement therapy (HRT) is a treatment used to alleviate symptoms associated with perimenopause and menopause by supplementing the body with estrogen and progesterone, hormones that naturally decline during this transition.
HRT has been in use for over seven decades, with its modern forms becoming widespread from the mid-20th century. It is primarily prescribed to relieve menopausal symptoms such as hot flashes, night sweats, vaginal dryness, and to prevent osteoporosis-related fractures.
Approximately 1-2 million women worldwide use HRT at any given time, though usage rates vary by country and cultural acceptance. In the United States and Europe, about 10-20% of postmenopausal women use HRT, with lower prevalence in many other parts of the world.
When Should I Start Hormone Replacement Therapy
The best time to start hormone replacement therapy (HRT) is during the perimenopausal period or soon after menopause begins, typically between the ages of 45 and 55. Starting HRT close to the onset of menopause can maximize symptom relief and confer cardiovascular and bone health benefits, a concept supported by the "timing hypothesis" that early initiation reduces risks compared to starting HRT many years after menopause.
Women going through premature or early menopause (before age 40 or 45) are also advised to start HRT promptly to protect against osteoporosis and cardiovascular disease until at least the average age of natural menopause. Although HRT can be started at any time when menopausal symptoms become bothersome, beginning it earlier in menopause generally offers safer and more effective outcomes.
Delaying HRT initiation many years after menopause may decrease its protective cardiovascular effects and increase certain risks, including stroke and thrombotic events, particularly if started after age 60. Therefore, healthcare providers recommend individualised evaluation and emphasize that the decision to start HRT should be a shared one, considering symptom severity, health risks, and personal preferences.
It is never mandatory to wait for severe symptoms or complete cessation of periods to begin HRT, and women experiencing troublesome symptoms should discuss early treatment options with their healthcare provider for optimal management (Australian Prescriber).
Relief of Menopausal Symptoms
Hormone replacement therapy (HRT) is the most effective treatment for relieving menopausal symptoms and in some countries including the UK and Australia it is known as the 'gold standard' in menopausal symptom treatment and relief.
It significantly reduces the frequency and severity of hot flashes and night sweats, improving sleep quality and overall comfort for many women. HRT can also alleviate vaginal dryness and discomfort, helping maintain sexual health and reducing urinary symptoms often associated with menopause.
Additionally, it may help with mood changes, joint pain, and other physical symptoms like headaches and skin changes that can occur during the menopausal transition. The relief of these symptoms with HRT often results in a better quality of life for women experiencing menopause.

Bone Health and Osteoporosis Protection
Hormone replacement therapy (HRT) is an effective treatment for preventing osteoporosis and reducing the risk of related fractures in postmenopausal women. Estrogen deficiency after menopause is a key factor causing bone loss and increased fracture risk.
Multiple studies and clinical trials, including the Women’s Health Initiative (WHI), have shown that HRT significantly preserves bone mineral density (BMD) at critical sites like the spine and hip, reducing the incidence of vertebral and non-vertebral fractures by approximately 30%.
The greatest bone-protective effects occur when HRT is initiated early in menopause, ideally before age 60 or within 10 years after menopause onset. HRT is recommended as a first-line option for osteoporosis prevention in women at risk, though it is generally not advised to start HRT solely for fracture prevention after age 60 due to potential long-term risks.
The protective benefit of HRT on bones wanes after discontinuation, so ongoing management or alternative treatments may be needed to maintain bone health long term. Women with early or premature menopause particularly benefit from HRT to prevent rapid bone loss.
While HRT’s bone benefits are well documented, current guidelines emphasize individualized treatment to balance fracture prevention advantages with other health considerations. Overall, HRT remains a valuable therapeutic option for managing menopause-related bone loss and reducing fracture risk in appropriate patients.
Cardiovascular Health
Hormone replacement therapy (HRT), when initiated within 10 years of menopause or before age 60, has been shown to provide cardiovascular benefits for women.
Observational studies and randomized trials indicate a consistent reduction in coronary heart disease incidence of around 30% in women who start HRT early in menopause. Estrogen in HRT promotes vasodilation, reduces cardiac fibrosis and oxidative stress, and improves lipid profiles, contributing to protection against atherosclerosis development.
This early initiation "timing hypothesis" is supported by trials showing slower progression of subclinical atherosclerosis and reduced cardiovascular events in younger menopausal women using HRT compared to placebo. However, HRT is not recommended for primary cardiovascular disease prevention in older women or those starting treatment late after menopause due to increased risks such as stroke.
Heart disease remains the leading cause of death in women worldwide, responsible for about 1 in 3 female deaths globally. Cardiovascular disease claims more lives annually than all cancers combined, underscoring the significance of effective prevention strategies like timely HRT use in eligible women.
The balance of benefits versus risks in using HRT for cardiovascular protection points to the importance of individualised treatment decisions, focusing on age, time-since-menopause, and personal health profile.
Improvement in Mood, Cognition, and Wellbeing
Hormone replacement therapy (HRT) can have beneficial effects on mood and cognitive function in menopausal women, although the extent of these benefits may vary. Recent studies, including the KEEPS-Cog trial, indicate that HRT started early in menopause does not result in long-term cognitive harm or significant improvement but may reduce depression and anxiety symptoms during treatment.
Some evidence suggests that estrogen, particularly 17β-estradiol, may help preserve brain regions involved in memory and executive function, potentially lowering risk factors associated with dementia. Observational studies also hint at a possible reduced risk of Alzheimer’s disease and cognitive decline in women who begin HRT close to menopause, especially among those with specific genetic profiles, although findings are not universally consistent.
Overall, HRT should not be considered a primary treatment for dementia prevention but may provide mood stabilization and some cognitive benefits when started at the appropriate time around menopause.
Other Health Benefits
In addition to the commonly known benefits of hormone replacement therapy (HRT) such as relief from menopausal symptoms and bone health improvement, HRT may also offer other important health advantages.
Recent studies suggest that HRT can help reduce joint pain and stiffness, improving mobility and physical functioning in menopausal women.
There is evidence indicating that HRT may favorably influence skin health by enhancing skin thickness, hydration, and elasticity, which tend to decline with age and estrogen loss.
Furthermore, HRT has been associated with better weight management and metabolic profile, potentially lowering risks of developing type 2 diabetes. For women who started HRT within 10 years of menopause, improvements in muscle strength and reduced muscle loss have also been observed, contributing to better overall fitness and fall prevention.
Overall, these additional benefits can contribute to improved quality of life and healthy aging beyond managing classic menopausal symptoms.
Urogenital Health
Hormone replacement therapy (HRT) provides significant benefits for urogenital health, particularly in addressing symptoms associated with the genitourinary syndrome of menopause (GSM).
Estrogen loss during menopause leads to thinning and drying of the vaginal and urethral tissues, which can cause vaginal dryness, irritation, painful intercourse, urinary urgency, frequency, recurrent urinary tract infections (UTIs), and stress urinary incontinence.
Vaginal estrogen therapy, a form of HRT, has been shown to effectively restore the thickness and elasticity of these tissues, improving symptoms and reducing the risk of recurrent UTIs by more than 75%.
Systemic HRT may also reduce some urinary symptoms though its effects on incontinence are variable depending on hormone type and delivery method. Overall, HRT plays a critical role in improving vaginal health and urinary function, significantly enhancing quality of life for postmenopausal women experiencing urogenital symptoms
Hormone Replacement Therapy & Libido
Hormone replacement therapy (HRT) can also have a positive impact on libido, which often declines during and after menopause due to hormonal changes.
Estrogen-based HRT improves vaginal health by increasing blood flow and lubrication, reducing discomfort during intercourse, which may help enhance sexual desire and satisfaction. In some cases, adding testosterone to HRT regimens can further boost libido, particularly for women who do not experience improvements from estrogen alone.
Studies have shown that HRT skin patches, delivering hormones transdermally, are often more effective in improving sexual function than oral forms. While HRT is not a guaranteed fix for all women, it frequently helps restore sexual vitality and improve overall quality of life related to intimate relationships. Any treatment should be personalized and discussed with a healthcare provider to balance benefits and potential risks.
Life Expectancy and Healthspan
Hormone replacement therapy (HRT) has been associated with an increase in life expectancy and longevity among postmenopausal women.
Large observational studies have demonstrated that women who use HRT, especially for long durations (15 years or more), experience a 10-15% reduction in all-cause mortality compared to non-users. For example, one study showed that long-term estrogen therapy users had a lower age-adjusted mortality rate, translating to an increase in life expectancy by nearly 1 to 2 years when started close to menopause.
This survival benefit is attributed to improvements in cardiovascular health, bone health, and overall quality of life. However, these benefits are most prominent when HRT is initiated early in menopause and used at an appropriate dose, emphasising the importance of timing (Menopause.org).
Is HRT Right for You?
When considering hormone replacement therapy (HRT), personal health history and family history are crucial factors in determining if it is the right choice. Healthcare providers carefully evaluate an individual’s overall health, including any history of hormone-sensitive cancers (such as breast, ovarian, or endometrial cancer), cardiovascular disease, blood clots, stroke, liver conditions, and uncontrolled hypertension.
Family history of these conditions may also increase risk. Additionally, factors like smoking, age, and metabolic health must be reviewed to ensure safety and effectiveness. This personalized approach helps minimize risks while maximizing the benefits of HRT, supporting safe management of menopausal symptoms and long-term health.
Consultation with a healthcare professional is essential to tailor treatment to each woman’s unique health profile and preferences.

Blood Clot Risk
In absolute terms, around 1 in 1000 women taking oral HRT tablets may develop a blood clot each year, whereas the risk with patches or gels is similar to that of women not using HRT. This difference is largely because oral HRT undergoes first-pass metabolism in the liver, which influences clotting factor production, increasing the risk of venous thromboembolism (VTE).
Among oral preparations, those containing conjugated equine estrogen combined with medroxyprogesterone acetate carry the highest risk, doubling the chance of blood clots (odds ratio ~2.1), while oral estradiol combined with dydrogesterone presents a much lower risk (odds ratio ~1.18).
In comparison, combined oral contraceptive pills, which are used by about 20-25% of reproductive-age women globally, increase the risk of blood clots about three to four times compared to non-users, translating to roughly 1 in 3000 women developing a clot per year.
Other factors such as older age, overweight, smoking, and genetic predispositions (e.g., factor V Leiden mutation) further increase blood clot risk with HRT. These findings highlight the importance of selecting the safest HRT formulation according to individual risk profiles and underscore why non-oral routes are preferred in women with elevated clotting risk, offering effective symptom management with minimized risks
Breast Cancer
Studies show that the slight increase in breast cancer risk associated with HRT is influenced by the type of progestogen used. A systematic review suggests that when estrogen is combined with oral micronised progesterone and taken for more than five years, there is some limited evidence of an increased risk.
That said, the actual risk is very low. Even with the older forms of progestogen, the level of increased risk is still less than the breast cancer risk linked to being overweight or drinking around two glasses of wine each day.
Importantly, with the use of body-identical estrogen and progesterone, which form the basis of most modern hormone replacement therapies, the risk is considered barely significant. This is why many experts now view today’s hormone replacement therapies as a safe and effective option for symptom relief, especially when compared to outdated studies that focused on older formulations.
Stroke Risk
Hormone replacement therapy (HRT) slightly increases the risk of stroke, particularly with oral formulations, but the overall risk remains low, especially in women under age 60.
Large studies including the Women’s Health Initiative (WHI) found that standard-dose oral HRT increases the relative risk of stroke by about one-third compared to non-users, primarily due to ischemic stroke. This translates to about 2 additional strokes per 10,000 women per year for those under 60 using HRT for five years, equivalent to one extra stroke per 1000 women treated over that period.
Importantly, transdermal HRT (patches or gels) at low doses has not been shown to increase stroke risk, offering a safer alternative for many women. Factors such as older age, hypertension, smoking, and history of cardiovascular disease further influence this risk. Women considering HRT should discuss stroke and other risks with their healthcare provider to weigh benefits against potential risks based on their personal health status.
Side Effects
It is common to need adjustments to the dose or timing of hormone replacement therapy (HRT) if side effects occur, particularly during the first few months of treatment.
Minor side effects of HRT can include breast tenderness, headaches, nausea, bloating, fluid retention, mood changes, leg cramps, or irregular bleeding, and these often settle within three to six months as the body adapts.
Most guidelines recommend giving HRT at least 2–3 months, sometimes up to six months before making changes, since many side effects are temporary; however, significant or bothersome symptoms should prompt a consultation earlier, as changing the dose, switching the hormone delivery method, or adjusting the regimen can often resolve these issues.
Regular communication with a healthcare provider is important to tailor HRT for best individual results and to ensure that the benefits outweigh any side effects or risks. (NCBI).
Not Suitable for All
Certain women may not be suitable candidates for hormone replacement therapy (HRT) due to increased risks associated with their medical history or current health conditions. According to the latest 2024 literature, HRT is contraindicated in women with known, suspected, or past estrogen-sensitive breast cancer, active or history of venous thromboembolism (deep vein thrombosis or pulmonary embolism), unexplained vaginal bleeding, untreated endometrial cancer, or untreated severe hypertension.
Women who have experienced a stroke or have uncontrolled risk factors for stroke or blood clots are also generally advised against systemic HRT use. Although transdermal estrogen may be safer for some with clotting risks, the decision must always be individualized. Additionally, caution is needed in women with other estrogen-dependent cancers or significant cardiovascular disease. These recommendations emphasize personalized risk-benefit assessment to ensure HRT is prescribed safely, ideally under close medical supervision, particularly in women over 60 or more than 10 years post-menopause (NCBI).
Context Matters
Only around 15% of women worldwide take hormone replacement therapy and this varies from country to country but the low uptake is thought to be attributed to fear around cancer and other risks that are often over stated when it comes to HRT, this is why context is necessary for women to understand their own relative risk.
Sedentary lifestyle, obesity, and excessive alcohol consumption significantly increase the risk of heart disease and certain cancers in women, according to the latest statistics. Cardiovascular disease (CVD) remains the leading cause of death in women globally, accounting for about 30% of female deaths annually, which is more than twice the number caused by all cancers combined.
Women who are physically inactive or sedentary have a notably higher risk of CVD-related mortality, with studies showing that just one hour per day of moderate-to-vigorous physical activity can reduce the risk of death from cardiovascular causes by up to 60%. Conversely, prolonged sitting and inactivity increase all-cause mortality risk by 12% and cardiovascular death risk by 30%.
Obesity compounds these risks, contributing substantially to heart disease and certain cancers, with mortality rates significantly higher among obese women. Additionally, consuming more than four alcohol units per week escalates the risk of cancers and cardiovascular diseases, with heavy drinking linked to increased stroke and heart attack incidences.
These statistics highlight the critical importance of maintaining an active lifestyle, managing body weight, and moderating alcohol intake to minimize the burden of heart disease and cancers in women.
Non-Hormonal Alternatives
For women who are not suitable candidates for hormone replacement therapy (HRT) or prefer not to use it, several alternative options are available to help manage menopausal symptoms.
Lifestyle changes such as maintaining a healthy weight, regular exercise, avoiding triggers like spicy foods, alcohol, and smoking, and using cooling techniques can help reduce hot flashes and improve overall well-being.
Psychological approaches like cognitive behavioral therapy (CBT) and relaxation techniques including yoga and meditation may also alleviate symptoms and enhance quality of life.
Non-hormonal pharmacological treatments include selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), which have been shown to reduce hot flashes and mood disturbances.
Other medications such as gabapentin and oxybutynin can also be effective for vasomotor symptoms.
Supplements to use in Menopause
Supplements can be a valuable addition to menopause management, supporting overall health and helping alleviate symptoms naturally. Key supplements such as calcium and vitamin D are essential for maintaining strong bones and reducing the risk of osteoporosis.
Magnesium supports muscle relaxation, improves sleep quality, and enhances mood stability. Phytoestrogens, found in soy and red clover, offer plant-based compounds that may gently mimic estrogen effects, helping to ease hot flashes and promote hormonal balance.
Additionally, omega-3 fatty acids contribute to heart and brain health, which are important during and after menopause. Many women also find that B vitamins and vitamin E aid in boosting energy levels and reducing stress.
When used thoughtfully and combined with a healthy lifestyle, these supplements can offer comprehensive support throughout the menopausal transition, complementing other treatments and enhancing quality of life. It’s always best to discuss supplement use with a healthcare professional to tailor choices to individual needs and ensure safety.
Why Collagen is Important in Menopause
Bovine grass-fed collagen is particularly beneficial during menopause as it provides essential support for bone health, skin, hair, nails, and gut health, all areas that can be affected by hormonal changes during this life stage.
Collagen is a major structural protein in the body, making up about 90% of bone matrix and playing a crucial role in maintaining bone strength and flexibility.
During menopause, collagen production naturally declines due to reduced estrogen levels, which can contribute to bone density loss and increased fracture risk.
Supplementing with high-quality bovine collagen peptides supports bone mineral density and may help reduce osteoporosis risk.
Collagen also improves skin elasticity, hydration, and firmness, helping to counteract menopausal skin dryness, fine lines, and wrinkles. Additionally, it nurtures the health of hair and nails by providing amino acids necessary for their growth and strength.
Bovine collagen contains type 1 and type 3 collagen, which also support gut lining integrity, aiding digestion and overall gut health, important as hormone fluctuations can impact digestive function.
Choosing collagen from grass-fed sources ensures higher quality peptides and fewer contaminants, providing optimal nourishment during the menopausal transition.
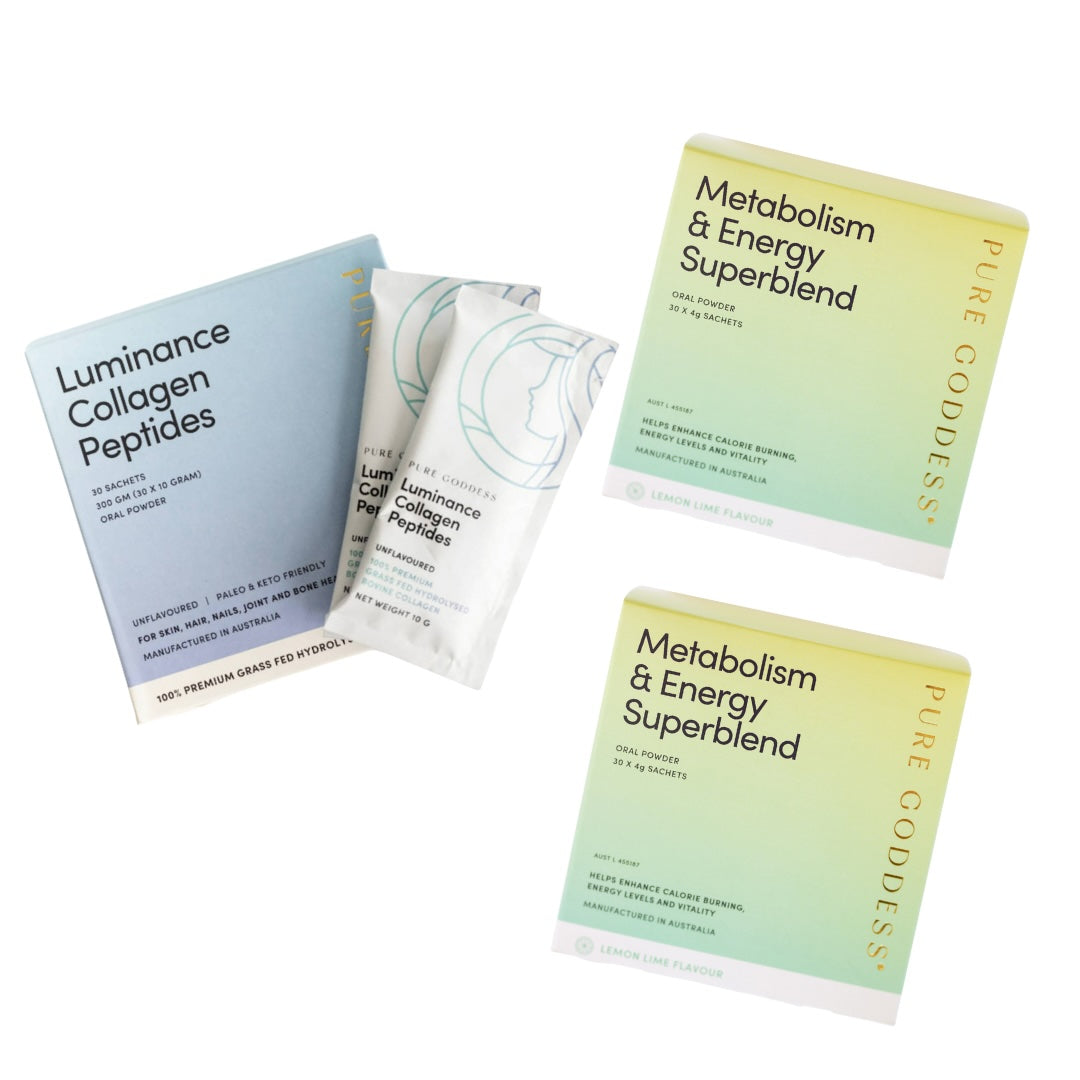
We created our very own Luminance Collagen Peptides because the benefits for perimenopausal and menopausal women are numerous, with bovine collagen helping to counteract and improve many of the symptoms.
Supporting Menopause With Nutrition
Good nutrition plays a vital role in managing health during menopause, with particular emphasis on fibre and protein intake. Fibre is essential for digestive health, helping to maintain regular bowel movements and prevent constipation, which can become more common due to hormonal changes.
It also supports heart health by helping to lower cholesterol levels and regulates blood sugar, reducing the risk of cardiovascular disease, especially important since heart disease risk increases after menopause.
Protein is crucial for preserving muscle mass and strength, which tend to decline with age and hormonal shifts, contributing to better metabolism and physical function. Including adequate protein from diverse sources such as lean meats, legumes, dairy, and plant-based options supports bone health and aids in weight management.
Balanced nutrition that emphasizes fibre and protein, combined with regular physical activity, helps women maintain overall well-being, energy levels, and reduces the risk of chronic diseases during and after menopause.

Targeted High Fibre Support With the Superblend
The Metabolism & Energy Superblend fibre supplement linked here is especially helpful during perimenopause and menopause as it supports key health needs during this transitional period.
Its blend of high-quality fiber promotes digestive health by maintaining regularity and supporting a healthy gut microbiome, which is crucial as hormonal changes can disrupt digestion and nutrient absorption.
The Metabolism & Energy Superblend also contains ingredients known to aid metabolism, helping to counteract the natural slowdown in metabolic rate that often occurs with aging and menopause. This supports sustained energy levels and weight management, which are common concerns for women going through these hormonal changes.
Additionally, the refreshing lemon lime or wild berry flavour makes it easy and enjoyable to incorporate into daily routines, ensuring consistent intake. Overall, this supplement provides a holistic approach to supporting digestive health, metabolism, and energy, all of which contribute to improved well-being during perimenopause and menopause.
To learn more about our Best Seller Metabolism & Energy Superblend CLICK HERE!
The Importance of Expert Medical Advice
Every woman’s menopause experience is unique, and HRT truly isn’t “one size fits all.” Before making treatment decisions, it is vital to seek expert medical advice from a healthcare professional experienced in menopause care. Shared decision-making ensures you thoroughly understand the benefits, risks, and options best suited to your health history and wellbeing. Clinicians can tailor the type, dose, and duration of HRT or non-hormonal support for you, provide ongoing monitoring, and adjust your plan as needed.
It’s equally important to remember that HRT knowledge continues to evolve as new research and large-scale studies are published. Staying up-to-date with expert sources ensures you have the most accurate, current information. Consulting a qualified specialist is the safest way to empower your menopause journey. Despite discussing risks and benefits within this blog, Pure Goddess do not and cannot provide individual medical advice. Please refer to your GP or menopause specialist.
Final Thoughts
Choosing HRT, supplements, or both is a personal choice best made in partnership with your healthcare team. Ask questions, weigh options, and schedule regular reviews to make the most informed decision. With the right support, menopause can become a phase of real strength and wellbeing.
This blog is informed by NICE and Australasian guidelines, Dr Louise Newson’s research and clinical guidance, and the latest expert publications on HRT and menopause care.



Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.